Deep research for healthcare claims - Kunle.app
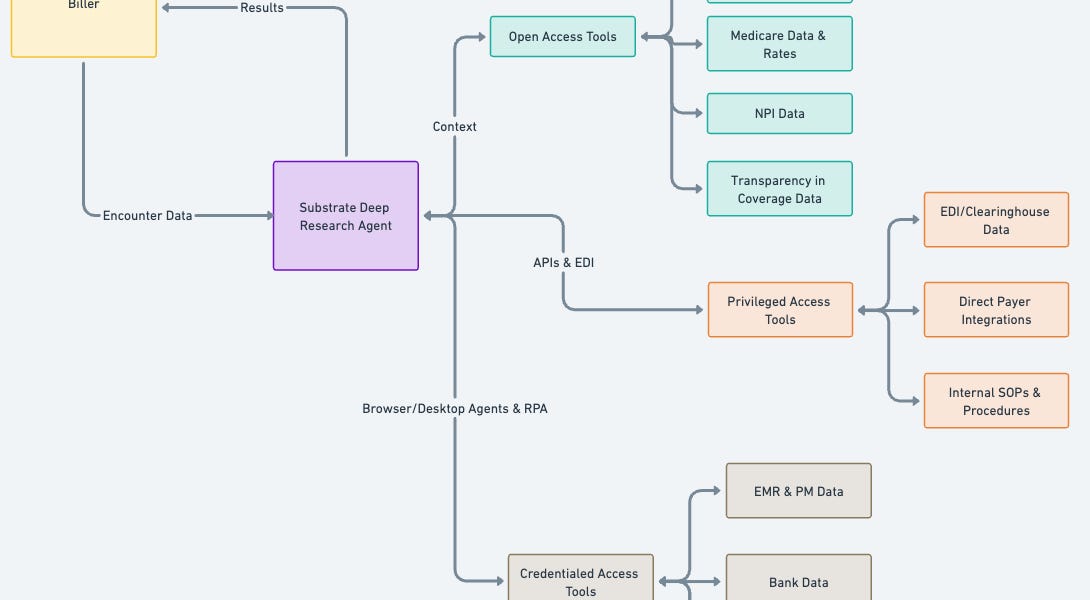
For the past year at Substrate, we’ve focused deeply on helping healthcare practices and billers get more efficient at AR follow up and denials management. While at Carbon I realized a frequent problem in AR is just understanding what is happening with a claim, or a queue/worklist of claims[1]. In the course of doing this, there are many different sources that a biller or RCM [2] operations team can use to get up to date. Some potential sources include:
Often, a biller only needs one source to tell exactly what is wrong and what to do next, but the exact source might differ from claim to claim or queue to queue, and they don’t know which one they need for a specific claim until they see it. For some encounters the claim status is sufficient, for others you might need an EOB or the correspondence document that was sent. Less often, the biller needs to triangulate across multiple sources to get to ground truth.
With this in mind, we began by building browser agents to navigate payer portals for practices. The first thing a biller does is look up the claim in the portal; this will often have either everything the biller needs or a pointer to where they should look (which would again be just another browser tab). Next, depending on what they learned, they’d potentially look in other places; checking the patient’s eligibility to figure out if there was another payer that the claim should have been sent to, checking the EOB for the claim to get the payment information, and more. Ultimately this information drives a decision about what to do next. This process is incredibly tedious; it’s a lot of copy-pasting data between tabs, waiting for payer websites to load, cross referencing information, and then reasoning about why the claim is in its current state. No one enjoys it, and it’s a massive time suck for billing & RCM operations teams. Some organizations have whole teams who only do this. In others, every team is responsible for logging into the portal and looking up the claim themselves.