Gut inflammation associated with age and Alzheimer’s disease pathology: a human cohort study
Scientific Reports volume 13, Article number: 18924 (2023 ) Cite this article
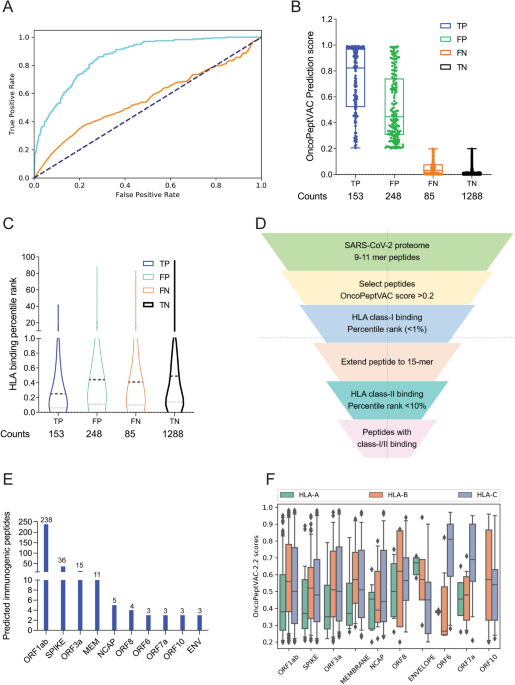
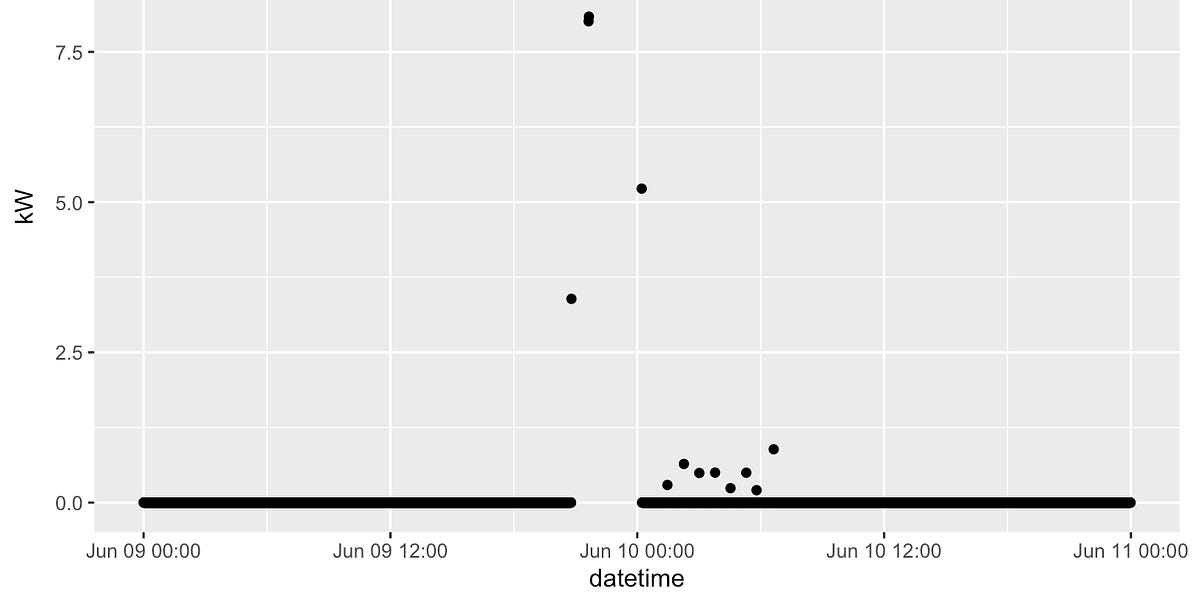
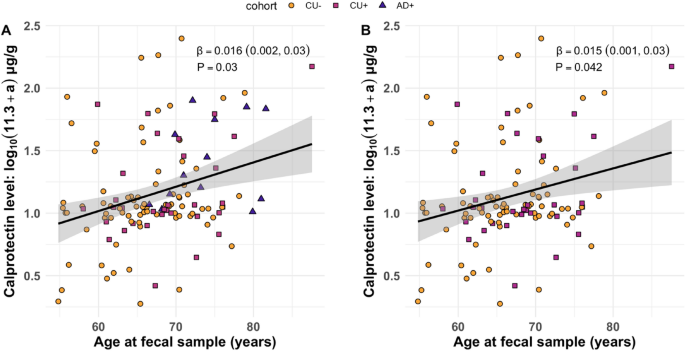
Age-related disease may be mediated by low levels of chronic inflammation (“inflammaging”). Recent work suggests that gut microbes can contribute to inflammation via degradation of the intestinal barrier. While aging and age-related diseases including Alzheimer’s disease (AD) are linked to altered microbiome composition and higher levels of gut microbial components in systemic circulation, the role of intestinal inflammation remains unclear. To investigate whether greater gut inflammation is associated with advanced age and AD pathology, we assessed fecal samples from older adults to measure calprotectin, an established marker of intestinal inflammation which is elevated in diseases of gut barrier integrity. Multiple regression with maximum likelihood estimation and Satorra–Bentler corrections were used to test relationships between fecal calprotectin and clinical diagnosis, participant age, cerebrospinal fluid biomarkers of AD pathology, amyloid burden measured using 11C-Pittsburgh compound B positron emission tomography (PiB PET) imaging, and performance on cognitive tests measuring executive function and verbal learning and recall. Calprotectin levels were elevated in advanced age and were higher in participants diagnosed with amyloid-confirmed AD dementia. Additionally, among individuals with AD dementia, higher calprotectin was associated with greater amyloid burden as measured with PiB PET. Exploratory analyses indicated that calprotectin levels were also associated with cerebrospinal fluid markers of AD, and with lower verbal memory function even among cognitively unimpaired participants. Taken together, these findings suggest that intestinal inflammation is linked with brain pathology even in the earliest disease stages. Moreover, intestinal inflammation may exacerbate the progression toward AD.
The gut microbiota is hypothesized to contribute to inflammaging, a condition characterized by chronic low-grade systemic inflammation without an acute driver such as infection, yet the physiological mechanisms by which this occurs remain poorly understood1,2,3,4,5. It is possible that age-related shifts in the composition of the microbiome produce an inflammatory environment within the intestine, which degrades the epithelial barrier. This may enable luminal bacterial components such as lipopolysaccharides and peptidoglycan fragments to enter systemic circulation and trigger a peripheral inflammatory response2,6,7,8. Evidence supports the barrier degradation component of this hypothesis, suggesting that gut permeability increases with aging and age-related diseases. For instance, levels of high-mobility group box 1 protein, which induces intestinal inflammation, are correlated with advanced age as well as markers of chronic inflammation, frailty, and impaired nutrient absorption9,10,11. Further, elevated permeability appears more frequently among older adults with inflammatory conditions including type 2 diabetes and irritable bowel syndrome (IBS)2,12. However, few intestinal permeability studies have been completed in healthy aging adults, and these studies have yielded inconclusive evidence, so it remains unclear whether elevated inflammation and permeability can occur prior to the onset of age-related disease.
Leave a Comment
Related Posts