Seven-year performance of a clinical metagenomic next-generation sequencing test for diagnosis of central nervous system infections
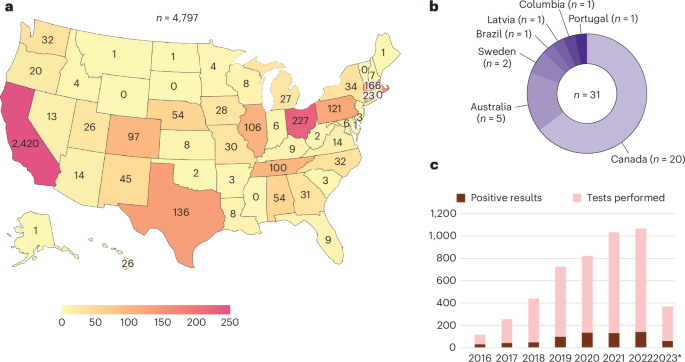
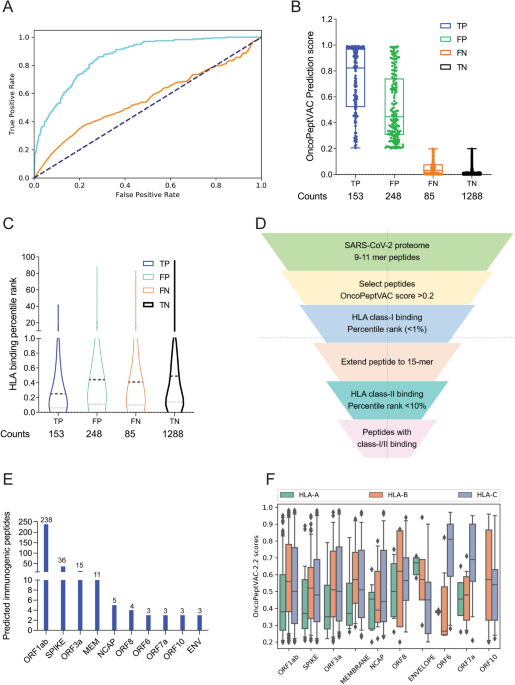
Metagenomic next-generation sequencing (mNGS) of cerebrospinal fluid (CSF) is an agnostic method for broad-based diagnosis of central nervous system (CNS) infections. Here we analyzed the 7-year performance of clinical CSF mNGS testing of 4,828 samples from June 2016 to April 2023 performed by the University of California, San Francisco (UCSF) clinical microbiology laboratory. Overall, mNGS testing detected 797 organisms from 697 (14.4%) of 4,828 samples, consisting of 363 (45.5%) DNA viruses, 211 (26.4%) RNA viruses, 132 (16.6%) bacteria, 68 (8.5%) fungi and 23 (2.9%) parasites. We also extracted clinical and laboratory metadata from a subset of the samples (n = 1,164) from 1,053 UCSF patients. Among the 220 infectious diagnoses in this subset, 48 (21.8%) were identified by mNGS alone. The sensitivity, specificity and accuracy of mNGS testing for CNS infections were 63.1%, 99.6% and 92.9%, respectively. mNGS testing exhibited higher sensitivity (63.1%) than indirect serologic testing (28.8%) and direct detection testing from both CSF (45.9%) and non-CSF (15.0%) samples (P < 0.001 for all three comparisons). When only considering diagnoses made by CSF direct detection testing, the sensitivity of mNGS testing increased to 86%. These results justify the routine use of diagnostic mNGS testing for hospitalized patients with suspected CNS infection.
Meningitis, encephalitis and/or myelitis associated with infections of the central nervous system (CNS) can cause severe and often life-threatening illness1,2. Timely diagnosis and treatment are paramount to improve clinical outcomes for these infections, and delays have been associated with increased morbidity and mortality3,4. A comprehensive infectious workup requires a combination of culture-based, serologic and nucleic acid amplification testing. However, it is estimated that the cause of meningoencephalitis remains unknown in approximately 50% of cases, which hinders clinical management and the initiation of appropriate and effective therapy5,6.







/cdn.vox-cdn.com/uploads/chorus_asset/file/23641763/acastro_220614_5290_0001.jpg)




/cdn.vox-cdn.com/uploads/chorus_asset/file/25735095/casio1.jpg)